Cow’s milk allergy
Cow’s milk is important for children as it provides essential nutrients for growth and development. When children are allergic to cow’s milk, it’s important to replace these foods with appropriate replacements. The following information will help you plan a menu and cater for children with cow’s milk allergy.

This resource is available as a downloadable file in following languages:
Key information
- Children with cow’s milk allergy are allergic to the protein in milk. They must avoid cow’s milk, dairy foods, and foods with cow’s milk as an ingredient. They must also avoid A2 milk, lactose free milk and lactose
free dairy products, sheep and goat’s milk. - Babies with cow’s milk allergy can drink expressed breast milk or cow’s milk free infant formula provided by their parents.
- Children with cow’s milk allergy must be offered milk alternatives with added calcium. Check with the child’s parents or carers which alternative milk or infant formula is suitable for them.
- Cow’s milk should not be removed, or banned, from the menu of a long day care centre for all other children who are not allergic. Cow’s milk contains important nutrients.
Providing food and drinks to children with cow’s milk allergy
This fact sheet is for cooks and chefs working in children’s education and care.
All food allergies must be taken seriously, and staff should know how to manage an allergic reaction. For information and guidance about managing food allergy, see the National Allergy Council Best Practice guidelines for anaphylaxis prevention and management in children’s education and care.
For more information on preparing and serving food for children with food allergies, complete the National Allergy Council All about Allergens for Children’s education and care course and download the All about Allergens for Children’s education and care booklet.
The Healthy Eating Advisory Service course Managing allergies and other dietary requirements in children’s education and care should then be completed. You will find a micro-module specific to managing cow’s milk allergy within this course.
Cow’s milk must be strictly avoided for children with cow’s milk allergy while attending an early childhood service.
Children who tolerate baked milk, or small amounts of milk as part of a medical allergy treatment program, should only be given those foods at home.
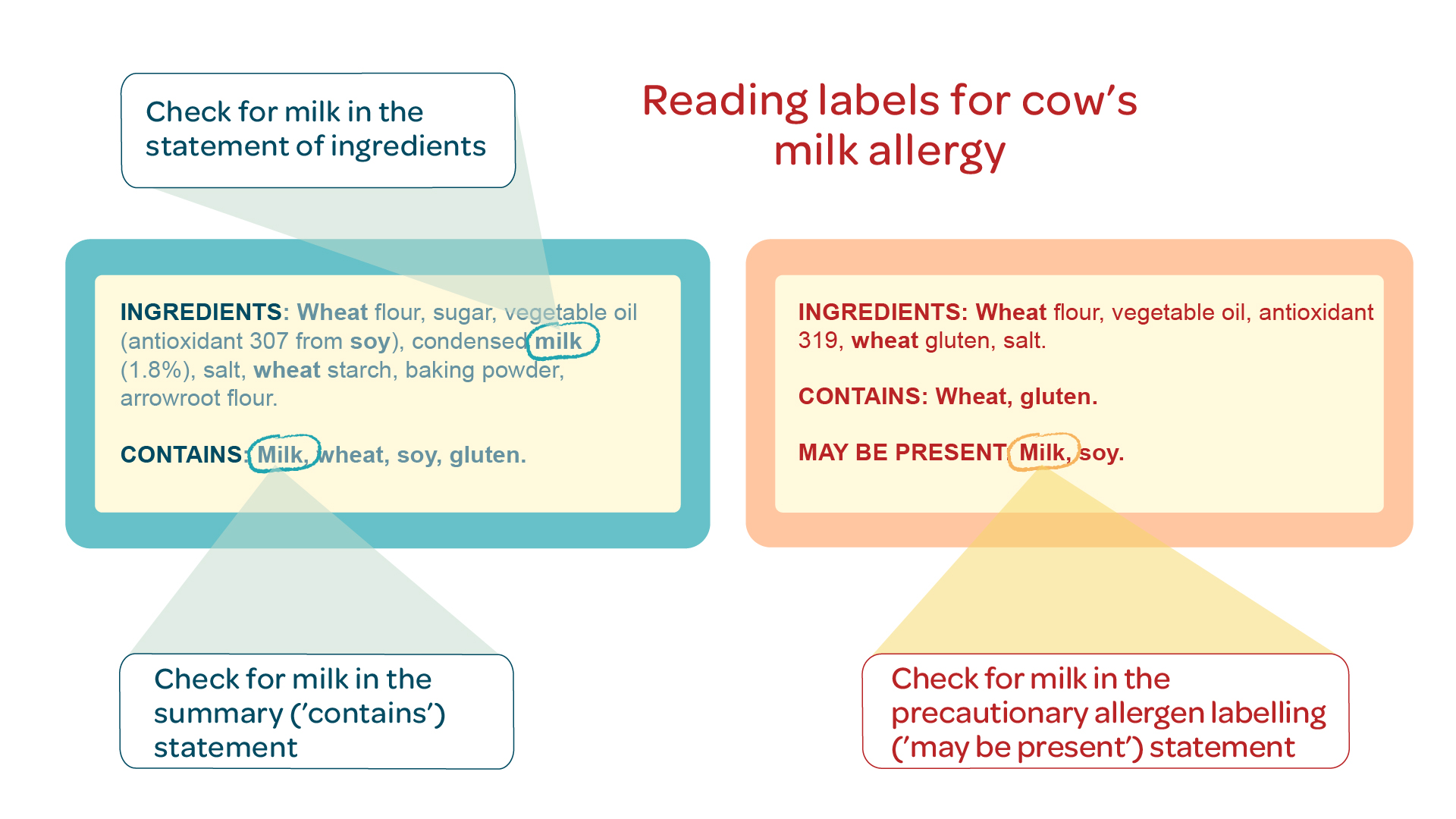
Reading food labels for cow’s milk allergy
It’s important to check the labels of all packaged foods for cow’s milk as an ingredient.
You should also check for precautionary allergen labelling for milk, for example ‘may be present’ or ‘may contain’ statements.
These products must not be given to children with
cow’s milk allergy.
If you notice a food does not have a label, ask the supplier for a product information form.
You should read food labels for milk as an ingredient each time you purchase the product, when it is delivered, and when you serve the food or before you use it in cooking for a child with cow’s milk allergy.
For more information, refer to the Reading food labels for food allergens section of the Food Allergy Aware website.
Cow’s milk allergy and lactose intolerance are different
Lactose free milk and lactose free dairy foods are not suitable for children with cow’s milk allergy.
Cow’s milk allergy can be life-threatening. Children with cow’s milk allergy are allergic to the protein in milk.
Lactose intolerance is not an allergy. Lactose free products have had the lactose, a type of sugar in milk, removed. Lactose free products contain milk protein and will cause an allergic reaction in children with cow’s milk allergy.
Foods and drinks that contain cow’s milk, or likely to contain milk as an ingredient, are listed below. Check the Menu planning guidelines for long day care for more information on foods to include on your menu as some of the foods listed as examples do not meet the menu planning guidelines.
| Food Group | Foods and drinks containing, or likely to contain, cow’s milk |
|---|---|
| Milk, yoghurt, cheese and/or alternatives | • Cow’s milk – regular, reduced fat, skim, A2, UHT, powdered, evaporated, condensed, buttermilk • Lactose free milk and other lactose free dairy foods • Sheep and goat’s milk • Regular and partially hydrolysed infant formula • Yoghurt, yoghurt drinks, custard • Fermented milk drinks • Cheese – cheddar, ricotta, cream, cottage, goats, sheep • Plant-based or soy cheese |
| Lean meats, poultry, fish, eggs, tofu, nuts and seeds, legumes/ beans | • Some meat patties, burgers, pasties, sausages, meatloaf • Fish fingers, chicken nuggets • Sausage rolls, pies • Processed meats, deli meats • Crumbed and battered foods • Egg dishes made with milk or cheese • Flavoured baked beans, for example cheese flavour |
| Grains (cereal) foods | • Bread with milk as an ingredient • French toast • Glazed bread products • Some breakfast cereals and muesli bars • Commercial baby cereals, teething rusks • Macaroni cheese • Filled pasta |
| Fruits and vegetables | • Fruit bars • Some canned vegetable soups • Commercial potato salad • Instant mashed potato |
| Cakes and biscuits | • Commercial and homemade cakes, biscuits, muffins, slices, pastries • Pancakes, pikelets • Waffles • Flavoured dried biscuits |
| Fats and oils | • Margarine • Butter • Ghee • Cream, imitation cream |
| Salad dressings and sauces | • Creamy salad dressings, for example coleslaw, Caesar, mayonnaise • Tartare sauce • Hollandaise sauce • Bechamel sauce • White sauce • Cheese sauce • Yoghurt sauce |
| Dips | • Commercial dips • Raita dip |
| Soups | • Creamed soups |
| Jams and spreads | • Nutella • Cream cheese spread |
| Drinks | • Milkshakes • Flavoured milk drinks • Chocolate drink powders • Malted milk powders • High protein drink powders • Drinking chocolate |
| Coconut products | Some coconut products including coconut drinks, juices, milk, and cream contain milk as an ingredient. Some are contaminated with cow’s milk, but this may not be shown on the label. Use coconut products with caution. |
Planning meals for children with cow’s milk allergy
Replacing cow’s milk on your menu
Cow’s milk contains protein, fat, energy, and calcium which are important nutrients for children’s growth and development.
Children with cow’s milk allergy need a milk replacement with similar nutrition to cow’s milk. The milk replacement you use must have at least 100mg of calcium per 100ml. Check with the child’s parents which milk or infant formula is suitable for them.
When replacing cow’s milk on your menu, remember to check if children have other food allergies and check that the replacement does not contain those allergens. Below is a list of suggested replacements to use in place of a cow’s milk.
Cow’s milk should not be removed from the menu of a long day care centre because it contains important nutrients.
Children who do not have cow’s milk allergy should continue to be served cow’s milk.
For more ideas, see the National Allergy
Council’s Ingredient Substitution Tool for foods you can use to replace cow’s milk.
| Cow’s milk product | Suggested replacement |
|---|---|
| Cow’s milk | • Soy milk • Oat milk • Rice milk • Almond milk Oat, rice and almond milk are low in protein and energy compared with soy milk. They are ok to use in cooking but not as a main milk drink. |
| Yoghurt | • Calcium-fortified plain soy yoghurt Most dairy free yoghurts are low in protein and calcium and do not meet the Menu planning guidelines for long day care. |
| Cheese | Nutritional yeast provides a cheese flavour to meals (for example on top of pasta, in an egg or tofu scramble). Cheese substitutes do not contain enough protein and calcium to meet the requirements of the Menu planning guidelines for long day care. You should therefore offer a glass of calcium-fortified milk alternative on the side of the meal as a replacement to cheese. Check with the child’s parents or carers which milk alternative is suitable for them. |
| Margarine | • Dairy-free margarine |
Cow’s milk alternatives must contain
at least 100mg per 100ml of calcium.
Always check food labels for cow’s milk
even if you have used the product before.
How to change recipes
Here are some examples of how to change recipes for cow’s milk allergy. If a separate meal is required, make meals for children with allergies look like meals served to the rest of the children. This way children with allergies will feel included at mealtimes. of suggested replacements to use in place of a cow’s milk.
| Recipe | Modification to recipe |
|---|---|
| Beef stroganoff | • Children with cow’s milk allergy: add calcium fortified plain soy yoghurt at the end • Children without cow’s milk allergy: add regular plain yoghurt at the end |
| Bolognese | • Children with cow’s milk allergy: add nutritional yeast at the end • Children without cow’s milk allergy: add regular cheese at the end |
| Lasagne | • All children: make the white sauce with calcium fortified soy or rice milk • Children with cow’s milk allergy: add nutritional yeast at the end instead of parmesan cheese • Children without cow’s milk allergy: add regular cheese at the end |
| Pikelets | • Use calcium fortified soy or rice milk instead of cow’s milk. |
| Custard | • Made from scratch with eggs and calcium fortified soy or rice milk instead of cow’s milk |
More information on our website
Menu planning and recipe modification for food allergies
Storing, making, and serving food for children with cow’s milk allergy
Children with cow’s milk allergy can react to very small amounts of cow’s milk in their food.
Make sure you have good food allergen management processes to prevent the risk of cross contamination from foods that contain cow’s milk.
This includes:
- cleaning surfaces and equipment
- storing food safely for allergies
- preventing cross contamination of food allergens during cooking and serving
- washing hands or changing gloves in between handling different foods.
More helpful resources and information
For more information see the National Allergy Council’s All About Allergens training for Children’s education and care and All about Allergens for Children’s education and care booklet, and the Healthy Eating Advisory Services e-learning micro modules on managing food allergies.
Further information and support
Healthy Eating Advisory Service:
- Early childhood services
- Recipes
- Menu planning guidelines for long day
care - Practical management of food allergies
and intolerances factsheetAllergy e-learning module: cow’s milk
allergy
National Allergy Council:
- All About Allergens training for Children’s
education and care - All about Allergens Resource Hub
(Children’s Education and Care section) - Preparing infant formula for children’s
with cow’s milk allergy (video)
For more ideas, see the National Allergy Council’s Ingredient Substitution Tool for foods you can use to replace cow’s milk.
For more information please phone 1300 22 52 88 or email heas@nnf.org.au
Except where otherwise indicated, the images in this document show models and illustrative settings only, and do not necessarily depict actual services, facilities or recipients of services. This document may contain images of deceased Aboriginal and Torres Strait Islander peoples. In this document, ‘Aboriginal’ refers to both Aboriginal and Torres Strait Islander people. ‘Indigenous’ or ‘Koori/Koorie’ is retained when part of the title of a report, program or quotation. Copyright © State of Victoria 2016
Written and reviewed by dietitians and nutritionists at National Nutrition Foundation, with support from the Victorian Government.
Featured Recipes
Explore all recipes
Register your interest
"*" indicates required fields